What is a basal cell carcinoma?
A basal cell carcinoma (BCC) is the commonest type of skin cancer. They are sometimes referred to as ‘rodent ulcers’ and account for about 80% of all skin cancers in the UK. There are number of different subtypes of BCC, and the treatment depends on the subtype. A Nodular BCC presents as a slow growing nodule and is the commonest form of BCC, accounting for about 60% of all cases.
What does a nodular
basal cell carcinoma look like?
Nodular BCCs can vary greatly in their appearance but often have pearl-like rim surrounding a central crater with blood vessels easily visible. People often first become aware of them as a scab that bleeds occasionally and does not heal completely. BCCs most commonly develop at sites of sun exposure on the central face, neck, ears, chest and back. 90% are situated in the head & neck area.

How is nodular basal cell carcinoma diagnosed?
Most nodular BCCs will be diagnosed clinically based on the appearance of raised nodule with some superficial blood vessels called telangiectasia. If the skin is stretched, the lesions often have a shiny pearly shiny border. If there is diagnostic doubt, a skin biopsy of the lesion can be taken following a local anaesthetic injection. In most patients, a skin biopsy is not required prior to treatment.

How is nodular basal cell carcinoma treated?
Surgical skin excision with stitches
The ‘gold-standard’ way of removing a nodular BCC is to excise the lesion following an injection of local anaesthetic. We would typically take margin of 4mm around the lesion in an elliptical shape and make length of the scar 2.5-3.0 times the width of the BCC. This allows the scar to be orientated in the correct position and edges stitched together to give the best outcome. Many patients are slightly surprised by the size of the scar but typically the wound heals well longer-term with a fine white scar that is very cosmetically acceptable.
For larger lesions on the face including those at difficult sites with poor movement of surrounding tissues, a skin flap or skin graft may be required. This would typically only be needed in 10% of patients needing surgery. Skin specialists are trained in all types of dermatological surgery and can discuss the best options with you when you are seen.
There are some videos to watch of skin if you would like to see the process. Patients may not choose to do this if they are squeamish of surgery!
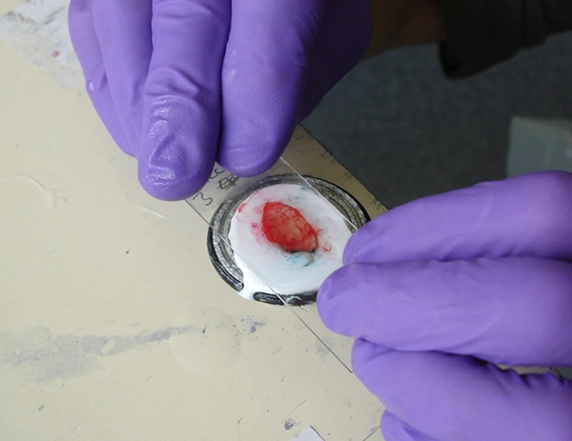
Excision involves the injection of local anaesthetic into the skin, which may cause discomfort for a few seconds. When the skin is numb, the area is removed as an ellipse of tissue. The scar is usually placed along a tissue relaxation line to achieve the best cosmetic result or hidden within normal skin folds on the face.
The skin tissue is sent for analysis to check whether it is free of skin cancer at the edges (results typically take 3-4 weeks). The edges are stitched back together and a wound dressing is usually applied. Stitch removal is necessary 7-10 days later at your primary care surgery. Wound care information is usually provided in writing with instruction of the does and don’ts following skin surgery.
Most patients who have had skin excisional skin surgery will have a permanent white scar that matures over a 4-6 months. The scar will normally be acceptable to most patients. The scar may stretch at sites such as the chest, back and shoulder.
Typical scars after excisional surgery – larger BCCs
Skin surgery side-effects
Side-effects include a risk of wound skin infection, bleeding of the wound, scarring, and occasionally disturbances to skin sensation. Wound infection is more commonly seen in patients having skin cancer surgery because the surface of the skin may be eroded and have growth of bacteria on it prior to surgery. You may be asked to take antibiotics in certain circumstances to reduce this risk. A raised red scar called a hypertrophic or keloid scar may develop following surgery at certain sites including around the inner canthus of the eye, shoulder, chest and back. These may necessitate a steroid injection and further clinical review.
Curettage and cautery
A conservative option to treatment in older patients, is to surgically remove the BCC by scraping if off following a local anaesthetic injection using a device called a curette. This produces a deeper scar that may heal as a white depressed indent in the skin that is slightly larger than the original skin lesion. This is a less aggressive option than conventional skin excisional surgery but does have a high rate of cure (80-85%). In younger patients, conventional excisional surgery is usually preferred because the rate of cure is higher (>95% and scar may be more acceptable.)
In patients with complex medical and/or social needs, curettage is a good alternative to excisional surgery and many patients find this to be a very acceptable treatment.
Typical scars after removal by curettage and cautery
Skin flaps and grafts
Patients with larger nodular BCCs may need a skin flap or skin graft to reconstruct the surgical wound area following removal of a BCC that is large or situated at a site of poor tissue movement such as the nose or lower leg. If this is required, it would normally be discussed with you prior to surgery.
The wound care following removal with a skin flap or graft may necessitate several visits to the clinic. There is also a higher rate of complications including skin infection.
Radiotherapy x-ray treatment
In older patients or those patients with high-risk tumours that are incompletely excised, radiotherapy may be offered as an option for treatment. There are two types of radiotherapy used. The first type is a very localised treatment called brachytherapy for smaller tumours. The second type of treatment is conventional radiotherapy that is spread over two-weeks or occasionally involves just 2 treatments.
Radiotherapy tends to be used in difficult skin cancers on the face. It can leave a white scar with red blood vessels longer-term and is typically used in older patients because the scars following radiotherapy can be unsightly after many years. Radiotherapy is only available at regional cancer centres and can only be used on a single occasion. It cannot be used on the lower leg or back because the wounds can take too long to heal.
Mohs micrographic surgery
This involves the excision of the affected skin that is then examined under the microscope straight away to see if all the BCC has been removed. If any residual BCC is left at the edge of the excision, further skin is excised from that area and examined under the microscope. This process is continued and repeated until all the BCC is removed.
Mohs surgery is very useful in larger BCCs that are at high risk sites that can not easily be removed by conventional surgery, or in those lesions with indistinct margins. A specific type of BCC called a morphoeic BCC may need Mohs surgery. Less than 2% of patients with a BCC will be recommended for this type of surgery in the UK.